Background
Plasmodium vivax, ovale, malariae, and falciparum (P. falciparum most virulent).
Disease initiated by the bite of a female anophelene mosquito.
Aneophelene mosquito originates from the tropical areas between 60° and 40°
A careful exposure history is necessary: country and area of travel, including stopovers, and date of return.
- ¾ reported malaria cases in UK = Plasmodium falciparum
- P. falciparum can lead to life-threatening multi-organ disease
- Most non-falciparum malaria cases are caused by P vivax (P ovale or P malariae are rare)
- Mixed infections with more than 1 species of parasite can occur
Clinical Features
Malaria should be suspected in anyone with a fever or a history of fever who has returned from or previously visited a malaria- endemic area, regardless of whether they have taken prophylaxis.
- Incubation period 6 days - 1 month
- May present more than 6 months later (P. vivax and P ovale)
No specific symptoms. Most have:
- Fever headache general malaise
- GI upset, jaundice or "pneumonic" symptoms uncommon
- Most missed malaria infections are erroneously diagnosed as non-specific viral infections, influenza, gastroenteritis or hepatitis
- Children are less likely to complain of chills, arthralgia/ myalgia or headaches
- No specific findings on examination
- Children may have hepato/splenomegaly
- Signs of hepatic de-compensation are late
Diagnosis
- Dx cannot be excluded until 3 blood specimens (thick and thin) have been examined by an experienced microscopist
- P. falciparum malaria can be diagnosed almost as accurately using rapid diagnostic tests (RDTs) which detect plasmodial antigens or enzymes
Consider
Other travel-related infections, e.g.
- Typhoid
- Hepatitis
- Dengue
- SARS
- HIV
- Meningitis/encephalitis
- Viral haemorrhagic fevers (VHF)
Investigations
Aside
- An acute attack of malaria does not confer protection from future attacks
- Chemoprophylaxis should be stopped on admission to hospital as this may interfere with parasite detection
All travellers returning from the tropics with a fever should have
- Thick and thin blood films (stained with Giemsa's stain) to ID species and % parasitised (98% sensitivity in expert lab.)
- The thick smear is most useful when there is low parasitaemia
- A single blood film may be falsely negative
- Not important to take blood during fever
- Full blood counts
- Repeated after treatment has been initiated to assess progress (anaemia)
- Platelet counts: may be low (If ≤50 x 109/L screen for FDPs and bleeding time to identify DIC)
- Blood glucose: exclude hypoglycaemia
- Blood cultures: septicaemia may be a complication of severe falciparum malaria
- Chest X-ray: shadows may indicate pulmonary oedema or adult respiratory distress syndrome
- Urine output, urea, creatinine: o assess dehydration and identify renal failure
- ABG (in severe cases): to assess pulmonary oedema / respiratory distress syndrome
Complicated falciparum malaria
- Impaired consciousness or seizures
- Renal impairment (oliguria < 0.4 ml/kg bodyweight per hour or creatinine > 265mmol/l)
- Acidosis (pH < 7.3)
- Hypoglycaemia (<2.2 mmol/l)
- Pulmonary oedema or ARDS
- Anaemia (Hb <8 g/dL)
- Spontaneous bleeding/DIC
- Shock (BP < 90/60 mmHg)
- Haemoglobinuria (without G6PD deficiency)
Treatment
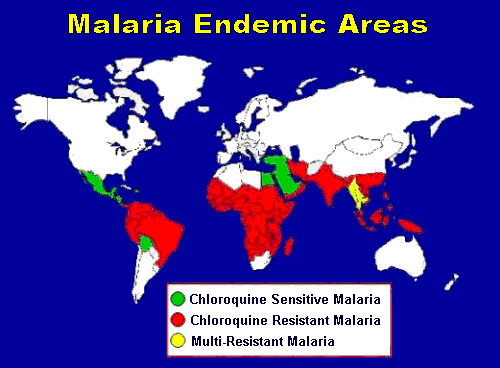
- Treatment of choice for non-falciparum malaria is a 3-day course of oral chloroquine. Dormant parasites (hypnozoites) persist in the liver after treatment of P. vivax or P. ovale infection: the only currently effective drug for eradication of hypnozoites is primaquine. Avoid in G6PD (triggers haemolysis)
- Uncomplicated P. falciparum malaria can be treated orally with co-artemether (Riamet), quinine or atovaquone plus proguanil (Malarone).
- Because it is so well tolerated, highly effective, and only a 3 day course is required co-artemether (Riamet) should be the firstline treatment for uncomplicated P. falciparum.
- Quinine is highly effective but poorly tolerated in prolonged dosage and is always supplemented by additional treatment, usually with oral doxycycline
- ALL patients treated for P. falciparum malaria should be admitted to hospital for at least 24 h (may deteriorate)
- Severe falciparum malaria, or infections with >2% of red blood cells parasitized, should be treated with IV quinine.
- Beware hypoglycaemia
- IV artesunate (ID consultant only) reduces high is useful in selected cases
Beware and seek complications:
- Some unwell patients may require haemodynamic support
- Please seek signs of impending ARDS, DIC, renal impairment or seizures
- Severe intercurrent infections (esp. gram negative bacteraemia) may be easily missed
Malaria in Pregnancy
Falciparum malaria in pregnancy is more likely to be severe and complicated: the placenta contains high levels of parasites.
The treatment of choice for falciparum malaria in pregnancy is quinine; doxycycline is contraindicated in pregnancy but clindamycin can be substituted for it, and is equally effective. Primaquine (for eradication of P. vivax or P. ovale hypnozoites) is contraindicated in pregnancy.
Malaria in children
May present with atypical e.g. GI upset or sore throat.
Children can be treated with most of the antimalarial regimens which are effective in adults, with appropriate dosage adjustment. Doxycycline plus quinine should not be given to children under 12 years but clindamycin can be substituted for doxycycline, and pyrimethamineesulfadoxine (Fansidar) may also be an effective substitute.