Vertigo
An illusion of motion where no motion exists (not to be confused with syncope/pre-syncope).
Seek details of:
- Onset
- Duration
- Repetition
- Hearing/tinnitus
- Headache
- Vomiting
- Diplopia
- Recent medication
Differentiate between central and peripheral vertigo, since the former are almost always a result of serious pathology
“Red flags” for posterior circ. stroke
- Sudden onset vertigo or disequilibrium with one or more additional posterior circulation symptoms:
- Headache
- Gait or limb ataxia
- Visual change (diplopia or field loss)
- Dysarthria, dysphagia
- Limb weakness
- Sudden onset vertigo or disequilibrium with a HINTS examination suggesting a central cause
- Hx migraine, presentation with any new posterior circulation symptoms, even if these occur with headache
Ask a senior to review if there are any two new acute onset posterior circulation symptoms (especially if there are risk factors for stroke) or any new focal posterior circulation neurological signs.
Clinical
Central
- Less intense
- Not positional
- Hearing rarely affected
- Nystagmus not ↓ by ocular fixation
- Brain stem /cerebellar signs
Hallpike (with central)
Should only be completed on patients with brief (<30 sec.) episodes and no vertigo/spontaneous nystagmus at exam. time.
- No latency of nystagmus
- Nystagmus non-fatiguing
- Multidirectional
- Vertigo lasts >1min
Peripheral
- Intense spinning / swaying
- Aggravated by position
- Altered hearing / tinnitus
- Horizontal nystagmus is unidirectional (unaffected by gaze direction)
- Nystagmus ↓ by ocular fixation
- Nystagmus fast phase worse looking away from damaged labyrinth
Hallpike (with peripheral)
- 2-20s latency
- fatigue with repeat testing
- unidirectional
- <1min
Pattern |
Nystagmus |
Typical causes |
Peripheral * |
Burst of upbeat-torsional nystagmus, lasting < 30 seconds, triggered by the Dix-Hallpike test to one side. Unidirectional spontaneous (i.e., primary gaze) nystagmus, with ↑ in velocity in the direction of the nystagmus fast phase and ↓ velocity in the opposite direction. E.g. left beating nystagmus in primary gaze, with an increase in velocity with left gaze, and a decrease (but not reversal) with right gaze. |
BPPV Vestibular neuronitis |
Central |
Spontaneous vertical nystagmus (upbeat or downbeat) Gaze-evoked direction changing nystagmus (i.e., persistent left beating on left gaze and then persistent right beating on right gaze) Persistent down-beating nystagmus triggered by a positional test such as the Dix-Hallpike test. |
Stroke MS Chiari malformation Meds: (e.g., antiepileptics) Cerebellar degen. disorder |
The Dix-Hallpike test should only be used for patients with short (30 sec) episodes of vertigo with head movement and no spontaneous nystagmus.
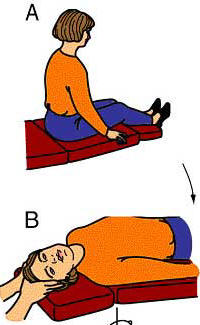
§ The Dix-Hallpike test is a specific positional test to asses for positional nystagmus. The patient sits upright and the head is turned about 45° to one side. The patient is then quickly guided by the physician down to a supine position with the head extended over the end of the examining table. In this position, the eyes are observed for nystagmus triggered by the test. The patient is then brought back to the sitting position and the test is then repeated with the head turned to the opposite side.
BPPV = benign paroxysmal positional vertigo.
* For peripheral vestibular nystagmus, the velocity of nystagmus typically increases by inhibiting visual fixation and decreases by encouraging visual fixation.
HINTS test
"Head-Impulse"-"Nystagmus"-"Test-of-Skew"
The patient must have ongoing vertigo & spontaneous nystagmus at the time of testing.
HI = Horizontal Head Impulse Test (h-HIT)
The HIT is abnormal with vestibular neuritis (nerve issue, so reassuringly, not a central lesion).
Abnormal is good! (in someone with vertigo).
HIT also normal in normal patient (so must only be interpreted in a patient who still has vertigo and nystagmus at the time of exam).
- Ask patient to look at your nose
- Rotate patient's head R and L 20° then rapidly back to mid-line
- Look for "catch-up" saccade
N = Nystagmus test
Check for nystagmus - primary (central) and lateral gaze (no fixation).
- Patients with AVS show a dominantly horizontal unidirectional (direction of nystagmus unaffected by changed in gaze direction) nystagmus, which beats only in one direction and ↑ in intensity when the patient looks in the direction of the nystagmus fast phase (AWAY from the offending labyrinth)
- Patients with a central cause may exhibit a change in the direction of eccentric gaze
TS = Test of Skew
A vertical ocular misalignment which results from an imbalance in neural firing when there is a central stroke/lesion.
- Patient looks at your nose
- Cover, then rapidly uncover one eye
- Look to see if the uncovered eye re-aligns vertically
- Repeat with other eye
Interpreting HINTS
Reassuring HINTS exam:
Must have all 3 of:
- Unidirectional nystagmus
- No vertical skew deviation
- Abnormal HIT but only in one direction
A dangerous HINTS:
Has any of the 3 below:
- Normal Head Impulse Test
- Direction-changing nystagmus
- Any skew deviation
The HINTS exam is more sensitive and specific than general neurological signs or than MRI in detecting medullary/pontine stroke.
Causes
Causes of central vertigo
- Cerebellar infarct/bleed **
- Brain-stem:
- CVA e.g. lateral medullary syndrome
- Other infarcts of caudal pons
- Neoplasm
- MS
- Trauma
Unilateral sensorineural loss needs tumour exclusion (ENT OPD). The whisper test with finger-rub distraction should be followed up with Rinne's and Weber's to establish basis of hearing deficit.
NOTE: - cerebellar haemorrhage suggested by acute ataxia and vertigo ± headache ± nausea and vomiting with no paralysis is a neurosurgical emergency and requires urgent CT & neurosurgical opinion
Peripheral causes of vertigo
- Meniere's: Triad of bouts of vertigo, tinnitus & progressive deafness
- Vestibular neuronitis: no hearing loss
- BPPV: particularly provoked by altered position
- Drugs:
- Aspirin affects the cochlea giving rise to tinnitus
- Aminoglycosides affect vestibular apparatus primarily
- Suppurative labyrinthitis: from recurrent otitis media / mastoiditis etc
- Acoustic schwannoma & meningioma: gradual onset, pre-ceded by hearing loss
Treatment
Peripheral features positive
- Stop triggering drugs if appropriate
- Chronic hearing loss - discuss with ENT
- If BPPV, use Epley manoeuvre(below)
- Other - brief course stemetil & GP review
- CUH Referral Vestibular Assessment / Mx
Central features positive
- Treatment as per cause
- Urgent MRI/CT if ? cerebellar lesion / base skull #
- Neurology review if ? MS
- Refer stroke team (CT "code stroke")if ? CVA
Drug treatment
- Stemetil 5mg tds, Antihistamines (e.g. cyclizine PO tds)
Links/References
- Newman-Toker et al. HINTS Outperforms ABCD2 to Screen for Stroke in Acute Continuous Vertigo and Dizziness. Academic Emergency Medicine. Volume 20, Issue 10, pages 986–996, October 2013
- Kattah JC, Talkad AV, Wang DZ, Hsieh YH, & Newman-Toker DE (2009). HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke; a journal of cerebral circulation, 40 (11), 3504-10 PMID: 19762709
- Babak et al. Application of the ABCD2 Score to Identify Cerebrovascular Causes of Dizziness in the Emergency Department. Stroke. 2012; 43: 1484-1489
- CUH Referral for Vestibular assessment and management