Background
Requirement to reduce blood pressure over hours (hi BP is causing end organ damage) rather than weeks. Remember that illicit drugs particularly cocaine may cause acute hypertension.
Signs end organ damage
- Encephalopathy (or stroke)
- Intra-cranial Haemorrhage
- Myocardial ischaemia/AMI
- Aortic dissection
- Acute heart failure
- Eclampsia
- Acute renal failure
Examine for:
- Lying & standing BP (volume status)
- BP both arms (aortic dissection)
- Heart failure
- Fundoscopy (haemorrhages, papilloedema, exudates)
- Neurological exam (lateralising signs / meningism)
Investigations
- ECG (ischaemia)
- Dipstick urine
- CXR (dissection or APO)
- U&E & Creat
- βHCG (eclampsia)
- ± CT Chest
- ± CT Brain
If end organ damage, goal is to reduce MAP by 25% in 1st hour then 25% over next 24 hours
MAP = [(Dia BP x2) + Sys BP] / 3
Treatment suggestions for hypertension with end organ damage
Acute renal failure / insufficiency
- Ca++ antagonists. Beware heart failure (clinical overload). Beware Hypovolaemia
Aortic dissection (aim for max Sys BP 110)
- β-blockers (Labetalol) first line ± nitrates
Heart failure or ischaemia
- GTN (SL and then IV), ACEI, diuretic if not hypovolaemic,β-blockers
Eclampsia
- β-blockers (or Hydralazine), sedation
Stroke or SAH
- Labetalol - please see management of hypertension in Stroke
Encephalopathy
- Nirtoprusside or Labetalol
| Agent | Dose | Indications |
|---|---|---|
| Sodium Nirtoprusside | Initially 0.5-1.5µg/kg/min. Titrate up in increments of 0.5µg/kg/minMax up to 8µg/kg/min | Hypertensive encephalopathy, Myocardial ischaemia, Pulmonary oedema, Aortic dissection (+ ß blocker) |
| Labetalol | Labetalol 10 to 20 mg IV for 1 to 2 min. May repeat or double every 10 min (max dose 300 mg). Then infusion 2mg/min, titrated as required | Stroke syndromes, Hypertensive encephalopathy, Aortic dissection, Phaeochromocytoma, Eclampsia |
| Nitrates | Isosorbide Dinitrate 2-10mg/hr max 20mg/hr. Glyceryl Trinitrate 10-20µg/min max 200µg/min | Cardiac ischaemia, Pulmonary oedema |
Initiation of treatment for patients WITHOUT end organ damage
 Only in exceptional circumstance should anti-hypertensive treatment be initiated in the emergency department (signs of end organ damage)
Only in exceptional circumstance should anti-hypertensive treatment be initiated in the emergency department (signs of end organ damage)- GP should confirm (> 140/90 mmHg) on at least two visits
- Routine ambulatory blood pressure monitoring is of unproven value
- Please ask GP to formally assess cardiovascular risk ± refer to OPD
- Formally assess their cardiovascular risk
- Accelerated (malignant) hypertension and suspected phaeochromocytoma require immediate referral
- GP may start medications in patients with :
- Persistent BP > 160/100
- Raised cardiovascular risk and BP > 140/90
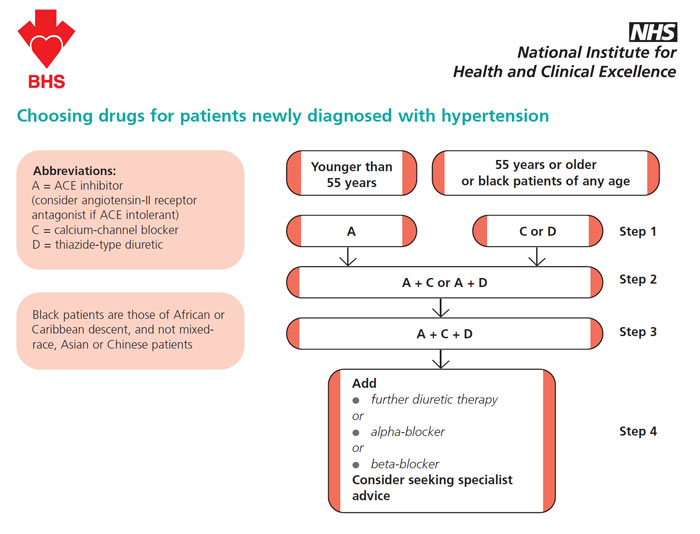
- In hypertensive patients aged > 55 or older or black patients of any age, the first choice drug should be
- Either a calcium-channel blocker or a thiazide-type diuretic
- In hypertensive patients younger < 55, the first choice for initial therapy should be
- An angiotensin-converting enzyme (ACE) inhibitor (or an angiotensin-II receptor antagonist if an ACE inhibitor is not tolerated)