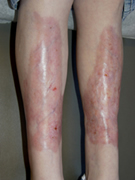

Necrobiosis lipoidica
- Inflammatory skin disorder of unknown cause
- Up to 75% of people who have NL will develop diabetes
- M : F = 1 : 3
- Classically asymptomatic (many insensate) and located pre-tibial or or medial malleolar areas
- Lesions are oval or irregularly shaped, indurated plaques with elevated margins with either red-brown or violaceous pigmentation. Gradually become brownish yellow with central depressed atrophy
- Treatment includes potent topical steroids, intralesional steroids Rarely systemic steroids
- Topical or injectable corticosteroids avoided if ulcers present

Acanthosis nigricans
- Reactive skin pattern
- Associated with endocrinopathy, malignancy (particularly GI) and some drugs
- Symmetrical hyperpigmented velvety plaques in the body folds
- Association between AN, obesity, hypertension, ischaemic heart disease and type 2 diabetes
- Generally two groups of patients:
- Type A is more common in young (particularly black) women with AN, primary amenorrhoea with hyper-testosteronaemia, virilisation, increased somatic growth, hyperglycaemia and hyperinsulinaemia with insulin resistance due to a congenital defect of insulin receptors
- Type B consists of patients who are older with features suggesting other autoimmune diseases, including raised ESR, proteinuria, hypocomplementaemia with anti-nuclear and anti-DNA antibodies
- AN is frequently asymptomatic, but lesions may become malodorous
- Treatment should be aimed primarily at weight reduction, keratolytics (e.g. topical retinoids) ± antibacterial soaps


Cutaneous infections associated with DM
No strong evidence to link diabetics with propensity to infection in general. But, some infections are more common and may be more severe in diabetics
Skin infections due to Staph aureus and group A Strep haemolyticus
- Folliculitis, furunculosis and abscess formation occur in people with poorly controlled diabetes
- Erythrasma (superficial infection of the skin at flexural sites) is due to the aerobic, Gram-positive Corynebacterium minutissimum
- Fungal infections encountered in patients with diabetes include dermatophytes (tinea pedis, onychomycosis), candidiasis (mucosal and cutaneous) and mucormycosis with necrotising nasopharyngeal infections
- Those at higher risk are patients with sensory neuropathy and peripheral vascular disease
- Onychomycosis (fungal nail infection) can damage surrounding skin and allow bacterial entry
- Often requires systemic anti-fungal therapy
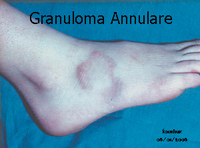
Granuloma annulare
- Unknown aetiology
- Ring of small, smooth, flesh-coloured or erythematous papules
- Dorsum of the hands, feet and fingers
Diabetic bullae
- Approx 0.5% of people with diabetes develop diabetic bullae (bullosis diabeticorum)
- Bullae occur spontaneously in adults
- Particularly long standing DM with neuropathy
- M > F, feet and lower leg
- Sometimes mildly painful or associated with a mild burning
- Heal in a few weeks without scarring
- Probably vascular aetiology
Diabetic dermopathy (shin spots)
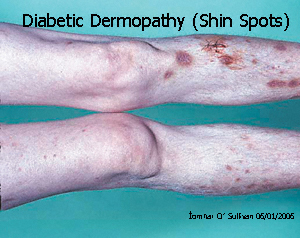
- Occur in up to 40% of people with diabetes
- Is the most common cutaneous manifestation of diabetes (not pathognomic.)
- Initial dull red papules, 0.5-1cm in diameter:
- Anterior aspect of the lower legs
- Generally bilateral and asymptomatic
- Evolve into crops of oval circumscribed, atrophic, slightly depressed, brownish lesions
- Spontaneously resolve, eventually healing with scar formation
- Probably due to microangiopathy
- Some studies have shown a significant correlation with other complications:
- Retinopathy, neuropathy and nephropathy
Diabetic thick skin (finger pebbles)
- Scleroderma-like skin change
- Thickening and induration
- Especially dorsum of the fingers
- Leads to clawing
- Correlation with angiopathy
‘Finger pebbles’ = multiple, tiny, flesh-coloured papules on the dorsum of the fingers, knuckle pads and periungual areas.
Scleroderma
- Poorly demarcated scleroderma-like induration of the
skin and subcutaneous tissue of the upper
back, neck and proximal extremities - Onset correlates with the duration of DM and with presence
of
microangiopathy
Eruptive xanthomas
- Widespread yellow to red papules
- Linear array in response to trauma
(Köbner phenomenon) - Poorly controlled DM who have massive hypertriglyceridemia
- Most commonly over
the buttocks, shoulders and extensor surfaces of extremities
Acquired perforating dermatosis
Kyrle’s disease (KD)
- Rare disorder of keratinisation
- Scattered or grouped keratotic
papules on the extremities and trunk - Frequently with renal failure