Background
- Acute torticillis = "twisted neck" (torus and collum). Sometimes present as "Wry neck"
- Child holds head tilted to one side, chin rotated to opposite side (unilateral muscle contraction)
Aetiology
- Trauma:
- Follow NICE Cx spine guideline (refer ortho)
- CNS symptoms: Headache, strabismus, diplopia:
- Ask a senior
- Infective:
- Constitutional/pharyngeal/URTI symptoms?
- Medications:
- Particularly dystonic meds (e.g. metoclopramide)?
Diagnostic approach to Paediatric Torticollis (Wry neck)
Neck stiffness after trauma
Potentialy life threatening causes
- Cervical fractures
- Mainly upper vertebrae, often alert on presentation, neurological signs rare. Immobilise and image
- Subluxation Cx spine
- More common than #. Can result from minor trauma.
- Commonest is rotatory altantoaxial subluxation (cord intact as transverse lig of atlas intact).
- Beware in children with Down syndrome - transverse lig very lax
- Sternomastoid (SCM) and neck tendernes localised to same side as head rotation. Contrary to inflammatory muscular torticollis (tender SCM is opposite to direction of head rotation)
- Open mouth peg view x-ray abnormal. Confirm with CT
- Refer orthopaedics - most treated with soft collar & NSAIDs
Potentially left threatening
- SCIWORA -(Spinal Cord Injury WithOut Radiological Abnormality)
- Ligament laxity in children. SCIWORA make up to 50% cord injuries in children
- Usually < 8 yo. Significant and / or progresive neulology up to 48 hours after trauma
- Admit all, even those with transient neurology as may remit and progress later
- Epidural haematomas of cervical spine
- Progressive neulology.
- Treat ABCs. Immobilise. Immediate neurosurgical opinion ± MR
Non life threatening
- Clavicular fracture
- Traumatic muscular contusion of neck
- Dx of exclusion only
Neck stiffness associated with infections / inflammatory conditions
Potentially life threatening
- Bacterial meningitis (see adult meningitis page)
- Children (especially infants) may presernt with torticollis rather than neck stiffness
- Retropharyngeal abscess
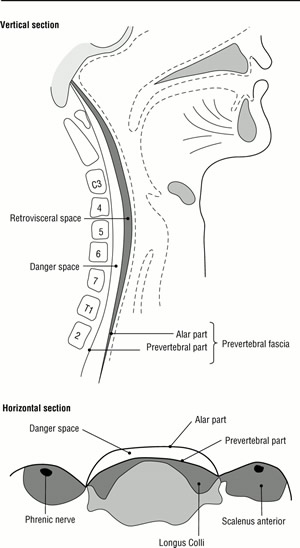
- Fever present - infection in space between posterior pharyngeal wall and anterior body Cx spine (see diagram )
- Commonest Gp A Strep, occasrinally Staph or anaerobes
- Clinically toxic, drooling, stridor
- Lateral neck x-ray may show soft tissue swelling
- Infections of the spine (osteomyelitis, abscess, discitis)
- More commonly occur in thoracic or lumbar spine
- Localised pain, fever, high ESR
- Usuall under 3 yo
- Usually bacterial (staph aureus) occasionally atypical, TB etc
- Local bone distruction, soft tissue sqwelling, reduced disc space on plain x-rays
- Bone scan may be positive before plain x-ray changes
Diagnostic flow diagram Fig 1 Fig 2

Generally non-life threatening
- Atlantoaxial subluxation from local inflammation
- Rheumatoid (Still's) arthritis, SLE, tonsillitis, phartyngitis or after ENT pocedures = Grisel's syndrome
- Sublux is rotatory, without displacement of atlas
- Usually neck pain and tender SCM, fever & dysphagia
- Head tilted to one side and rotated to side opposite the facet dislocation
- Plain x-rays may be normal, CT best to visualise (Most commonly no ant displacement of axis )
- If severe - early neurosurgical opinion
- Rheumatoid (Still's) arthritis, SLE, tonsillitis, phartyngitis or after ENT pocedures = Grisel's syndrome
- Cervical lymphadenitis
- Tender swelling over lateral aspect of neck ± fever
- Usually local S. aureus or strep, occasionally atypical e.g. TB
- Intervertebral disc calcification (IDC)
- Uncommon, self limiting, calcification of nucleus pulposus. Cause unknown
- Usually present with 1 - 2 days neck pain, torticollis, ± fever
- ESR usualy raised. WCC up in 1/3
- May require LP to exclude meningitis
Neck stiffness and CNS space occupying lesions (SOL)
Potentially life threatening
- Brain tumours - posterior fossa commonest site for childhood brain tumours
- Check for raised ICP, cranial nerve (particularly eye signs), lateralising or long tract signs
- Spinal cord tumours
- Astrocytoma typically caues pain at tumour site and neulological signs (incl. sphincter symptoms)
- Patients may hold their heads in forward flexion ("hanging head sign")
- Urgent MRI
- SOL of head / neck
- Nasopharyngeal carcinoma may present with epistaxis, neck pain and cervical adenopathy
- Others include acoustic neuromas, orbital tumours, mets, Arnold-Chiari malformations, AVM and syringomyelia
Generally non-life-threatening
- Benign tumours of head & neck
- Osteoid osteoma (older children and adolescents). Symptoms worse at night. Plain x-rays diagnostic
Congenital causes of Neck Stiffness
- Congenital muscular torticollis
- Aetiology unclear, probable birth trauma, SCM haematoma with resultant scarring
- Often palpable mass in inferior part of SCM. Mass not at birth but appears in neonatal period
- Head held with chin pointing away from affected, contracted SCM
- Associated craniofacial asymmetry(contralateral flattening of occiput and ipsilateral depression of malar prominence)
- X-ray to outrule other causes. Treat with passive stretching of affected muscle
- If deformity persists more than 6 months, may need surgical release (< 5%)
- Skeletal malformations
- Commonest is Kippel-Feil (congential fusion Cx vertebrae) may have atlantoaxial instability
- Scoliosis develops in 50%
- Classical triad (<50%) is limited neck ROM, low hairline and short neck
- Atlantoaxial instability
- Down synd., Kippel-Feil, other skeletal dysplasias, os odontoideum, Morquio syndrome mucopolysaccharidopsis)
- Benign paroxysmal torticollis of infancy
- Episodes of torticollis in association with pallor, agitation and vomiting
- Onset at 2 - 3 months, remits by 2 - 3 years
Miscellaneous causes torticollis
- Ophthalmologic, neurologic and /or vestibular causes (check visual acuity and exclude diplopia in all)
- Myaesthenia gravis (torticollis, ptosis, extra-ocular eye muscles and cranial nerve palsies
- Sandifer syndrome (torticollis, gastro-oesophageal reflux and hiatus hernia present as FTT and vomiting)
- Pneumomediastinum (usually after bout coughing or retching)
- Spasmus nutans (I bet this one is new to you too):
- Acquired torticollis, nystagmus and head nodding
- Become symptomatic in first 2 years
- Rarely underlying brain tumour (CT all), most benign self limiting condition
- Dystonic reaction (diphenhydraminbe 1 mg/kg will be diagnositc and therapeutic)
Links
- IAEM National Guideline: Torticollis. 2021. Drs Jessica Abrahams, Carol Blackburn, Mr John Russell, Mr Pat Kiely
- Fleisher G. Textbook of Paediatric Emergency Medicine. Lipppincott Williams & Wilkins
Content by Dr Íomhar O' Sullivan. Last review Dr; ÍOS 4/03/25.