Initial management facial injuries
Airway
- Foreign bodies
- Loose pieces of denture, teeth, bone may obstruct
- Remove dentures (please note if ? inhaled/ingested, some dentures are not radio-opaque)
- Keep any fragments of bone/teeth in sterile saline
- Haemorrhage - usually good suction only needed
- Postnasal haemorrhage may need packing
- Backward displacement of maxilla can obstruct airway
- Poor tongue support in mandibular fractures can cause airway obstruction
Examination
Eyes
- PERL
- Shape of pupil
- Vision present, clear or blurred
- Diplopia, extraocular muscles
- Subconjunctival haemorrhage
- Chemosis
- Conjunctival lacerations or abrasions
- Level of globes enophthalmos or proptosis
Bony margins
- Inspect and then palpate
- Look from front, side but also from above for malar flattening
- Palpate over nasal bones, orbital margins, malar and zygomatic arch, body of maxilla, condyles, ramus and body of mandible
Nasal CSF leak or CSF otorrhoea
Soft tissues
- Record swelling, bruising
- Record lacerations and / or incisions
- Check for foreign bodies
If at risk check parotid duct
Check trigeminal & facial nerve
Intraoral examination
- Occlusion, step deformities
- Loose and/or missing teeth
- Laceration, bruising
- Tongue stability and movement
- Difficulty in opening or closing mouth, deviation of chin on opening and closing
Referral guidelines
- Refer significant facial injury to the Maxillofacial Registrar on call in CUH
- Please confirm OPD (maxillofacial Team CUH) arrangements with patient in writing
Mandibular fractures
Mandible - considered to be a long bone bent in the middle and articulating with the skull via the temporomandibular joints. This arrangement means that there are natural points of weakness.
X-rays
OPG as initial film [BestBets].
If no # on OPG, request PA, lateral oblique and Towne's.
OPG (when available this is usually the only film required).
Common mandibular fractures
One or both condylar necks.
- Symphysis and one or both condylar necks
- Angle of mandible and the opposite angle or condylar neck
- Lower canine area and opposite angle or condylar neck
Examination
- "Pathognomic" = mal-occlusion or sublingual haematoma
- Inspection - deformity, swelling, bruising, lacerations over bone inability to open or close mouth, deviation of chin on opening or closing = derangement of dental arch or occlusion, missing or loose teeth/bone fragments/denture- lacerations or bruising especially in floor of mouth
- Palpation - steps along mandibular border, localised tenderness, tenderness and lack of movement of the mandibular condyles, anaesthesia over the distribution of the mental nerve
Referral
- Refer significant facial injury to the Maxillofacial team
- Analgesia
- PO antibiotics - Co-amoxiclav or metronidazole
- Soft diet
- Please confirm OPD arrangements with patient in writing
Dislocated jaw
- Spontaneous or secondary to yawning or blow with mouth open
- Confirm by x-ray
- Reduce by placing thumbs (wrapped in gauze) in retromolar fossa each side and fingers over chin. Get patient to relax - diazemuls if necessary. Press thumbs down and back and fingers upwards
- OPD
Zygomatic facial complex (malar) fractures
Imaging
Plain films are the imaging modality of choice.
CT is indicated for:
- Clinically unstable (le fort) injuries
- Those with eye symptoms/signs
- Mal-occlusion
Often from direct blow.
Examination
Inspection:
- Flattening or downward displacement
- Look from above to check symmetry of malar prominences
- Subconjunctival haemorrhage - lateral with no posterior limit
- Bleeding from one nostril
- Enophthalmos
- Interference with mandibular movement (depressed zygomatic arch catches on coronoid process of mandible)
Palpation:
- Orbital margins - palpable steps
- Widening at front zygomatic suture
- Infraorbital anaesthesia, and/or upper teeth
- Tender/bruised upper buccal sulcus
Management
No signs of retrobulbar haemorrhage
- Co-amoxiclav or erythromycin
- Patient instructed not to blow nose
- Refer significant facial injury to the Maxillofacial team
- Please confirm OPD arrangements with patient in writing
Signs of retrobulbar haemorrhage
- Beware proptosis / visual loss
- Record visual acuity in all
- Immediatey discuss with ED senior
- Inform ophthalmology & plastics teams
- If advised, refer to the Maxfax team
- Institute medical management before transfer
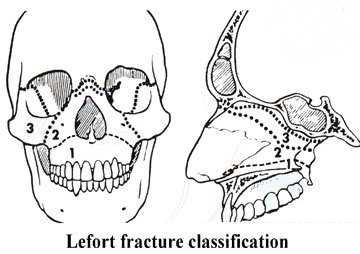
Middle 1/3 fractures (Le Fort I, II, III)
The maxilla is a complex bone made up of strong buttresses but with areas of weakness around the maxillary sinus.
Le Fort I
Transverse # through floor of maxillary sinuses (only palate moves).
Le Fort II
Through nose lower orbits and maxillary sinuses (pyramidal shaped #).
Le Fort III
Through orbits (craniofacial dysjunction) (separates the entire midface from the base of the skull).
Combinations occur and fractures are often comminuted.
Examination
Inspection
- Displacement: lengthening of the midface, bruising, lacerations
- Subconjunctival haemorrhage, enophthalmos, diplopia
- Bleeding/CSF from nostrils, or post-nasally
- Disruption of occlusion or dental arch
- Missing or loose teeth- bruising in centre of palate or buccal sulcus
Palpation
- Rock maxilla against stable point e.g. upper basal skeleton
- Check orbital margins for palpable steps
- Check infra-orbital nerve
x-rays
- 15 & 30 degree occipitomental (OM) views
- Lateral view facial bones
Blow out fracture
Involves the floor (or med walll) of orbit usually without the orbital rim. Usually caused by blunt objects hitting front of eye, e.g. squash ball.
- Enophthalmos and diplopia are early signs & "blackeye"
- Infra-orbital nerve paraesthesia
- Later, tethering of the inf rectus (or medial rectus) muscle - inability to look upwards on the affected side
- Record Visual Acuity in all
- X-rays - OM and submentovertical views:
- (SMV often not done initially, involves neck extension and left until neck status is certain)
- "Blow out" fracture gives the appearance of a teardrop in the maxillary antrum
Immediate referral to plastics SHO if visual symptoms
- Traumatic diplopia in children is a medical emergency. An ocular muscle may be caught in a "trapdoor" orbital fracture (usually inferior or medical wall) and requires emergency decompression to prevent ischaemia
- Blindness or visual symptoms are early warnings of a retro-orbital haematoma. Retro-orbital haematoma is a medical emergency. Please discuss with your Plastics Reg or your Consultant before imaging (most imaging not necessary - requires immediate decompression)
Plastics soft tissue referral if no eye symptoms / signs.
- Local policy is for routine antibiotic cover [BestBets]
- PO co-amoxiclav ± topical fucithalmic
- Refer significant facial injury to the Maxillofacial Registrar
- Please confirm OPD arrangements with patient in writing
Further Management
- Mx or most udisplaced fractures is conservative and CT scanning is not required
- Mx of those with any eye involvement is surgical (requires CT unless sight loss - immediate Sx)
- Mx most orbital fractures >10mm (even if undisplaced) is surgical (prevent late enophthalmus)
Frontal Bone fracture
Displaced, no neurological deficit:
- Refer significant facial injury to the Maxillofacial Registrar on call
- Please confirm OPD arrangements with patient in writing
Undisplaced, no neurological deficit or LOC or risk intracranial haemorrhage
- Review next plastics clinic (discuss with on call team first)
>Neurological deficit
- Seek neurosurgical advice
Nasal bone fractures
Clinical Dx - do NOT x-ray unless a FB is suspected.
There is no evidence for early manipulation of nasal fractures [BestBets].
Discharge if:
- No changes in the appearance of the nose
- No septal haematoma
- No septal cartilage dislocation
- Patient is happy with the shape of the nose
ENT in 5/7 if
- Deformity / pain
- Nasal obstruction
No septal haematoma, swollen difficult to assess or deformity
- Review ENT or MaxFax in 5-7 days
Septal haematoma
- Immediate referral to Maxillofacial or ENT SHO
Naso-ethmoidal fracture
Immediate referral to plastics SHO(discuss ENT review first).
Dental On-Call Cover for CUH ED
- Dental cover is separate from plastics cover
- A Dental SHO is on-call from home via switch. They are covered by a dental consultant on call from home. They will be happy to give advice or come in to see the following
- Trauma to the teeth
- Bleeding from tooth sockets
- Facial swelling associated with dental infection
- The dental SHO should not be called for toothache
OPD referrals
All dental / maxillofacial trauma follow up in Cork should be with the CUH maxillofacial surgeons or plastic surgery soft tissue clinic.
For visitors from Dublin, who must unfortunately leave Cork (against all logic or desire), the St. James Hospital referral form should be completed.