Background
- X-ray to look for avulsion fracture (better chance of healing)
- With a large fragment check that the DIP joint is not subluxed
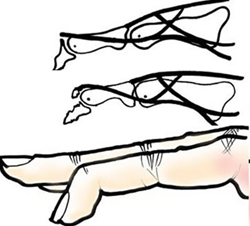
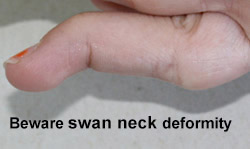
- A small percentage of patients develop hyperextension of the PIPJ (old volar plate injury or lax ligaments or "dominant middle slip"). This hyper extension must be corrected (splint PIPj in neutral also) if present. (Please see swan neck deformity below)
- In children, beware a Seymour fracture (peri-epiphyseal # DP) - see below
Management
- For the majority, general management includes : Apply a mallet splint full-time for 6 weeks, then at night for 2 weeks. GP follow up
- If there is still a lag as patient begins to mobilise at 6 weeks, place back into splint for a further 6 weeks
- If splint is removed the finger must be kept straight
- Explain the prognosis - (½ left with deformity even if in splint) but that the function of the hand / finger will not be effected
- Warn the patient that it may not heal
- Patients with exceptional hand requirements should be referred to the plastics clinic
- It is important that the mallet splint allows for full flexion at the PIP joint and patients are encouraged to mobilize at the PIPJ
- If the joint is subluxed please refer to the on-call orthopaedic or discuss with the plastics team Referral form
- If a Seymour # (avulsion of a nail bed/germinal matrix) causes a SH 2 physeal injury) is suspected, antibiotics are indicated. Seymour # may need ORIF (today) if fracture does not stay reduced when in splint (check x-ray after manipulation)

Prone to osteomyelitis.
Mallet Advice
- The stack splint will hold the DIPJ at 0° / neutral
- Ensure the patient can move the PIPJ to full extension and flexion
- Immobilisation of the PIPj can lead to complications
- If the patient is unable to flex the PIPJ fully either trim the splint or report it on the referral form
All patients should be given an advice sheet.
Mallet injuries >25% bony fragments should be referred to the VTAC in CUH (Amber). Others may be referred for the GP to follow up in 6 weeks, or to the plastics clinic.