Spinal injuries referral CUH
- All cervical injuries (± neurological involvement) should be referred to the neurosurgical team on call
- All thoracic and lumbar fractures (± neurological involvement) should be referred to the Orthopaedic team on call
Beware of injury to the spine (unconscious patient)
Prioritise A(with Cx spine control), B and C
- Apply stiff neck collar, sand bags and tape to help immobilise the cervical spine
- Request CXR, lateral view of the cervical spine and pelvis as a minimum in the ED
- To help reveal the C7/T1 junction, apply caudal traction on the arms to the limit of comfort when the radiograph is taken. Other radiographs may be taken later in the X-ray Department if the patient is stable
- Perform basic neurological examination
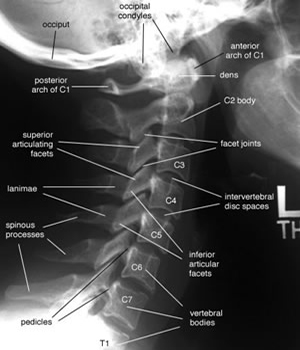
- Examine the lateral cervical X-ray which is usually adequate for revealing signs of significant trauma
- Alignment
- Fractures, dislocations (produce anterior displacement)
- abnormal separation of spinous processes
- prevertebral haematoma
- increased atlanto-odontoid gap (3mm in adult, 5mm in a child)
- AP and open-mouth views of the odontoid may need to be taken later in the X-ray Department
- If you can't see C7/T1 request a swimmer's view
- Thoracolumbar x-rays should be performed on all patients with multiple injuries or an accident mechanism with sufficient force that thoracolumbar injury could occur. A wedge fracture of thoracic vertebra may not be detected on log roll.
The conscious patient
Neck
- Place head in neutral position, if deviated (Stop if pain worsens or neuro.symptoms develop)
- Restrict movement (collar, sandbags, tape/vac. mattress)
- Note pain - site, radiation, neuro. symptoms, e.g. numbness & weakness
- Full neurol, exam. (include sacral reflexes if evidence of cord injury)
- Obtain lateral cervical radiograph C1 - C7/T1 ± caudal arm traction
- If C7 T1 junction still unclear, request CT
Check for:
- Mal-alignment
- Fractures
- Dislocations (producing displacement)
- Abnormal separation of spinous processes
- Prevertebral haematoma
- ↑ atlanto-odontoid gap (3 mm in adult, 5 mm in child)
- C1 - C3 spinolaminar alignment
- CT or AP and open-mouth views of the odontoid must be taken at some stage
- If there are neuro. symptoms or signs & x-rays are abnormal or the patient remains in significant pain, refer to the ED duty doctor (see clearing the cervical spine)
For more labelled x-ray please see Radiology.
C-spine lateral

Types of cervical spine fractures
Injury by mechanism
Hyperflexion injury (46-79%)



Hyperextension injury (20-38%)



Flexion rotation injury (12%)
Vertical compression (12%)
Lateral flexion / shearing (4-6%)
Location (by frequency):
C2,C6 > C5,C7 > C3,C4 > C1. See:
Cervical sprains (Whiplash)
Correlate history & examination when deciding whether or not to x-ray patients with neck sprains. Higher velocity, fall from a height, vertebral tenderness and neurological symptoms (ASIA Form if neurological signs) are the more important indicators for x-ray. If all radiographs and neurology are normal and the patient can mobilize well, treat with NSAIDS and refer to GP (Please see clearing the cervical spine section). Arrange review in ED or physiotherapy if concerned. Early mobilization in neck sprains speed recovery [Bestbets]. Please provide all patients with verbal and written advice about neck sprain. Referral to a chiropractor is not indicated [BestBets].
Thoracolumbar injuries
- Enquire about level of pain, radiation and neurological symptoms (e.g. numbness, weakness) ASIA Form if positive
- Perform chest, abdominal and neurological examination
- "Log-roll" patient to examine spine and localise tenderness
- Obtain CXR&CT if thoracic spinal injury
- Obtain AP and lat. X-rays - if patient otherwise stable
- Refer if unstable injury, burst fracture (see below) or abnormal neurology (please record on ASIA Form)
- Patients with stable fractures may be sent home with analgesia to rest but admit if unable to stand or lack of support at home. Fracture Clinic follow-up should be requested
- Beware of HYPERtension which may indicate autonomic dysreflexia
NB: Unstable injuries are associated with dislocations or fractures resulting in separation of the anterior and posterior vertebral complexes (e.g. fractured pedicles). The more common stable injuries are confined to simple wedge or crush fractures of the vertebral bodies and fractures of the transverse or spinous processes. A burst fracture is an unstable comminuted fracture of the vertebral body with posterior displacement of fragments which may impinge on the spinal cord. Compression fractures are associated with fracture of the os calcis produced by falling from a height.
Emergency treatment of cord injury
Options
- Surgical decompression
- High dose steroids
Aim
- Reduce secondary injury
- Improve motor fxn and sensation
- Reduce extent of permanent paralysis
Surgery
- Open wounds require surgical exploration
- Timing of surgery (closed cord injury) is controversial
- Surgically remediable cord compression due to dislocation of a vertebral body or displaced bone fragment must be treated urgently (within 2 hours)
- Even stable injuries can be associated with significant cord compression and may benefit from decompression surgery
- Early decompression has also been advocated for incomplete lesions, especially if the motor signs progressive
Steroids
- Use in spinal cord injury still controversial
- Mater Hospital Spinal Unit in Dublin advise against steroids in acute spinal cord injury
- Some early motor improvements are not maintained and ↑ sepsis, gastritris, pancreatitis (links below)
Links
- ASIA Form
- Paediatric radiology cases
- Autonomic Dysreflexia
- Sultan I et al. The safety and efficacy of steroid treatment for acute spinal cord injury: A Systematic Review and meta-analysis. Heliyon. 2020 Feb 19;6(2):e03414. doi: 10.1016/j.heliyon.2020.e03414. PMID: 32095652; PMCID: PMC7033344.