Background
When a patient arrives in the department with a painful condition - Think analgesia, reasurance, sling, immobilise, local anaesthesia, narcotics.
Do not send any patient away without some pain relief. You may only have to suggest they use the simple analgesics they have at home or can buy at a chemist.
- Mild pain - paracetamol or an NSAID [Not in active PUD or Aspirin sensitive patients]
- Moderate pain - a combination of the above two drugs
- Severe pain - add Opioid analgesics (Dihydrocodeine 30 mg)
It is worth asking asthmatics whether they have taken NSAIDs before. You may wish to look at NNTs for oral analgesics.
For children
Please refer to paediatric doses and paediatric pain management. For skin wounds in children, topical anaesthesia should be used in preference to lignocaine infiltration [BestBets]. Use TAC in preference to EMLA for topical anaesthesia [BestBets]
Analgesia for severe pain
The safest and most effective way of providing adequate analgesia is to administer small quantities of diluted morphine intravenously.
For paediatric patients and information on intranasal fentanyl please see paediatric analgesia section.
Local Anaesthesia
Toxic dose for Lignocaine is 3 mgs / Kg
(20 mls of 1% Lignocaine for 70kg adult)
- The dose in a child is 1 ml of 1% plain Lignocaine for each year of the child's age
- LA are best administered with the patient supine
Infiltration for local anaesthetics
- Use as small a needle as possible
- Begin proximally
- Inject slowly
- Repeat process distal to the wound
- Wait for > 5 minutes
Mx of Severe Local Anaesthetic Toxicity Signs of severe toxicity
Signs
- Periorbital/speech changes (unmyelinated c-fibres)
- Bizarre behaviour
- LoC, ± convulsions
- CVS: ↓HR, conduction blocks, asystole &VT
Immediate management:
- Stop injecting the LA
- Call for help
- Maintain airway, 100% oxygen
- Ensure adequate lung ventilation
- Confirm or establish IV / IO access
- Control seizures: with BDZ
- Assess cardiovascular status throughout
Mx of cardiac arrest assoc. with LA:
- Start CPR using standard protocols
- Manage arrhythmias using the same protocols
- Prolonged resuscitation may be necessary
Lipid emulsion:(70kg)
- IV/IO bolus of Intralipid® 20% 1.5 ml/kg over 1 min (100 ml)
- Start IV infusion of Intralipid® 20% at 0.25 ml/kg/min (400 ml over 20 min)
- Repeat the bolus injection twice at 5 min intervals if necessary (x2 further boluses of 100 ml)
- After another 5 min, ↑ the rate to 0.5 ml/kg/min if necessary (400 ml over 10 min)
- Continue infusion until stable and well perfused
- Continue CPR throughout treatment with lipid emulsion
- Recovery from LA-induced cardiac arrest may take >1 hr
- Please report all cases to the Irish Medicines Board and the LipidRescueTM
Nerve block
- Very effective method of providing analgesia, esp. in the upper limb
- You must wait longer than direct infiltration for the block to work as the anaesthetic must diffuse into larger nerves
- If the patient experiences pain in the nerve distribution then stop injecting immediately, withdraw slightly and try injecting again
- Avoid Adrenaline around end arteries e.g. digital, nose, ear or penile blocks
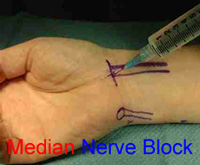
Median nerve block
- Median nerve lies between flexor carpi radialis and palmaris longus
- 1 to 2 cm proximal to distal flexor crease
- Aim under palmaris longus
- 4 - 5 mls 1% solution plus or minus Adrenaline
- If resistance - stop
- If swelling - correct
- A further 1 to 2 mls over subcut. tissues may be needed
Intercostal block
- Good for # ribs 6,7,8 (does not block visceral pain which requires coeliac plexus block)
- Contra-indicated where PTX would be dangerous (e.g. already reduced respiratory reserve)
Paravertebral block
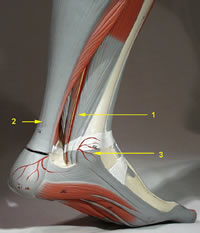
Tibial nerve block
- For the sole of the foot
- Use 10 ml of 1% lignocaine ± Adrenaline
- Do not use Adrenaline in patients with peripheral vascular disease
- Aim medial to the tendo Achilles behind the posterior tibia artery, between the tendons of flexor digitorum longus and flexor hallux longus
Supra-orbital/supra-trochlear block.
Is used for forehead and scalp anaesthesia. The supra orbital nerve leaves the orbit through the supra orbital notch. This notch lies medially in the supra orbital rim, on a vertical line through the medial aspect of the cornea. The supra-trochlear nerve exits the orbit at the junction of the superior orbital rim and the medial wall of the orbit. The two nerves have a sensory distribution from forehead to coronal suture from mid-line to temporal region.
Infiltrate subcutaneously completely parallel to the supra-orbital rim above the eyebrow 5 ml of 2% lignocaine with Adrenaline. Do not infiltrate directly around the nerve or its foramen.
Links
- IAEM Clinical Guideline: US-guided Erector Spinae Plane Block .... Mx Rib fractures in the ED. C D Vecchia, P Bullman, E Turcuman, C McDermot. 2023
- http://drgdh.wordpress.com/2011/06/24/fascia-iliaca-block-for-fractured-neck-of-femur-do-you-you-should/
- http://www.youtube.com/watch?v=4wJPkA073cg&sns=emhttp://www.ultrasoundpodcast.com/2012/03/episode-24-femoral-nerve/
- ESRA/ASRA statement 2018 - Regional Anesthesia in the Patient Receiving Antithrombotic or Thrombolytic Therapy: