Background
- Rare
- Cerebrovascular dysregulation due to acute BP changes and endothelial dysfunction
- Blood-brain barrier disrupted → white matter vasogenic oedema
- Most commonly in patients with pre-eclampsia/eclampsia or end stage kidney disease
- Chemotherapy, immunosuppressive agents and illegal drugs ↑ the risk
- Also seen in SLE and solid organ transplantation
- Mean age 57 years, 72% are women
Clinical
Presentation
- Hypertension
- Encephalopathy
- Headaches and/or seizures
- Classic imaging findings
Signs/signs
- Encephalopathy (94%) (delirium, drowsiness, fluctuating consciousness)
- Headache (up to 50%)
- Seizures (75%)
- Visual disturbances (up to 40%)
- Acute, severe ⇑⇑BP
| Disorder/condition | Specific |
|---|---|
| Systemic disorders | Renal failure, 1° aldosteronism, sepsis/shock, phaeochromocytoma |
| Pregnancy related | Pre-eclampsia, HELLP |
| Autoimmune Connective tissue; |
SLE, scleroderma, Sjögren's synd., vasculitis, IBD, crypglobulinaemia, Hashimoto's thyroiditis, many vasculitides |
| Post-procedural | Transplantation, IG transfusion, blood transfusion, spinal or vascular surgery |
| Haematological | Sickle cell, HUS, TCP, AML, ALL, non-Hodgkin's lymphoma |
| Metabolic | Porphyria, 1° Hyperparathyroidism |
| Neurological | Neuromyelitis, carotid dissection |
Differential Dx
- Posterior circ. ischaemic stroke
- Watershed infarcts
- RCVS
- CNS infections
- Demyelination
- Brain neoplasm
- Venous sinus thrombosis
- CNS vasculitis
- Mitochondrial disorders
Investigations
- CT may be normal
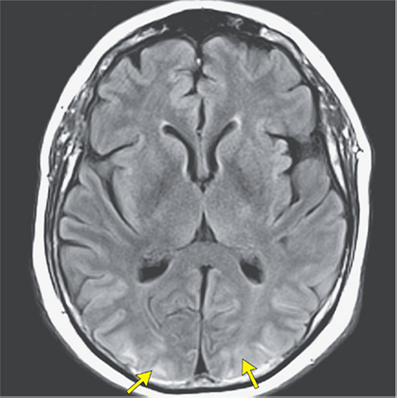
- MRI may show bilateral white-matter vasogenic oedema particularly in the occipital and adjacent parietal lobes (best seen on FLAIR sequence)
- MRI findings resolve after weeks-months in 70% of cases
- PRES can result in transient DWI abnormalities, haemorrhage or established ischaemic stroke
- Vessel imaging (MRA/CTA) may show diffuse or focal vasoconstriction with vasodilation ("string of beads" pattern)
- No specific blood tests
Management
- Early identification and treatment of the triggers for PRES (e.g. eclampsia, drugs)
- Consider admission to ICU particularly if BP, GCS or seizures are unstable
- Mainstay: BP and seizure control
- Lower BP slowly (max 25% reduction in the 1st hour)
- Titrate IV Labetalol
- Mx of pre-eclampsia/eclampsia in conjunction with obstetrics
- Seizures should be treated with anti-epileptic drugs
- Admit under stroke team
- Close monitoring for signs of worsening cerebral oedema and ↑ICP → urgent neurology review
Links/References
- Geocadin RG. Posterior Reversible Encephalopathy Syndrome. N Engl J Med. 2023 Jun 8;388(23):2171-2178. doi: 10.1056/NEJMra2114482. PMID: 37285527.
- Labetalol infusion preparation