Background
Anaemia, ↓platelets, anaemia:
- Variable signs and symptoms of end-organ ischaemia (arteriolar thrombosis)
- M = F
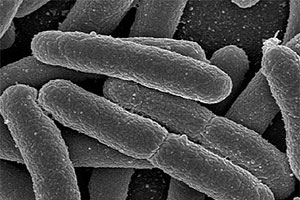
- Infective HUS (also known as diarrhoea-associated HUS or D+HUS) is recognised as a sequel to infection primarily with two gastrointestinal pathogens: Verocytoxigenic Escherichia coli (VTEC1) and Shigella dysenteriae
- Verocytotoxigenic Escherichia coli (VTEC1), or the pathogen responsible for the large outbreak of gastroenteritis in Germany in 2011 that produced 4000 cases of illness, of which more than 800 developed haemolytic uraemic Syndrome (HUS) and 50 died
- VTEC1 is highly transmissible; it can be spread from person‐to‐person, through food and water and from surfaces
- The infectious dose is tiny
- Ireland has one of the highest notification rate of VTEC (incidence rate of 12.16/100,000) in Europe with a high incidence of HUS (10%). 3% of HUS cases die. All of these HUS cases were admitted to hospital for extensive supportive measures
- HUS is the commonest cause of acute renal failure in children.
- Severity of the acute illness, especially the presence of CNS symptoms, is strongly associated with poorer long‐term outcome
- Other rarer causes of HUS include pnemococcus, HIV, CMV, EBV and influenza. Very rarely hereditary or acquired acquired complement dysregulation
Clinical
Triad of:
- Thrombocytopenia
- Non-immune (microangiopathic) haemolytic anaemia
- Acute renal failure
Presentation
- 1/7 vomiting then diarrhoea (±bloody) then more lethargic/aneuric as diarrhoea resolves
- Weakness, Lethargy, Pallor
- ↓ urinary output, oedema
- Purpura, Epistaxis
Differential Dx
- DIC
- Gastroenteritis
- HELLP Syndrome
- Henoch-Schonlein Purpura
- Intussusception
- Sepsis, Bacterial
- Thrombocytopenic Purpura
- TTP (TTP smilar but more severe encephalopathy, low levels of ADAMT13 and is rare in children)
Investigations
- ARF (↑↑ Urea & Creat)
- Urine +ve for prot / RBC
- D-Dimers normal
- FBC = Schistocytes (red cell fragmentation), †Hb (↑Retics) , ↓platelets (normal PT / APTT)
- Coombs test negative
- ↑LDH (normal PT / APTT)
- Blood cultures negative (toxic causes disease, not bugs)
- Stool cultures positive (MC&S)
- CT brain if seizure
Management
- Aggressive ARF management (esp. ↑K+, ↑BP), initially with fluid resuscitation
- Avoid nephrotoxic drugs (e.g. NSAIDs , gentamicin)
- ± correction U&E abnormality
- Urgent nephrological opinion
- Admit paediatrics (all will be transferred to neonatal ITU)
- Seizures (up to 30%) made more likely if ↑BP so hypertensive Mx crucial (discuss with paed. renal team but nifedipine 0.5mg/kg reasonable starting point), ±dialysis
- Notify public health
Note:
- Antibiotics have no role in shiga toxin E Coli HUS and in fact may worsen the disease process if given during the bloody diarrhoeal phase of illness. Azithromycin appears to be safe however
- Pneumococcal associated HUS needs treatment with a 3rd generation cephalosporin (Dx after leaving ED)
- Some consider plasma exchange (no evidence but it is of proven treatment for TTP which is difficult to exclude early in the disease process
Prognosis (E coli related HUS):
- Mortality approx 3-4% from CNS injury (eg cerebral oedema/infarction), sepsis, GI necrosis, ↑K+
- A further 5% have serious morbidity eg stroke or end stage renal disease
- 70% recover completely (the remainder varying renal dysfunction)
Links
- Health Protection Surveillance Centre
- Department of Public Health, HSE – South, Floor 2, Block 8, St. Finbarr’s Hospital, Douglas Road, Cork