Remember analgesia.Always assess and record the patient's ability to bear weight
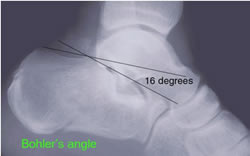
Fracture calcaneum (os calcis)
- May occur from a fall onto the heels or with "simple" inversion ankle injuries
- If in doubt - request axial X-ray
- If the sub-talar articular surface is involved, refer to the on-call Orthopaedic Team for admission
- Gross disruption of the subtalar joint is indicated by a flattening in Bohler's angle (should be 30° - 40°)
- If there is no sub-talar involvement apply a well padded POP backslab, advice, no weight bearing and provide crutches
- Elevate
- Consider prophylactic anticoagulation (LMWH) particularly if high risk of VTE or prior DVT.[BestBets]
- Arrange a Fracture Clinic appointment
- Warn patient to return immediately if pain increases
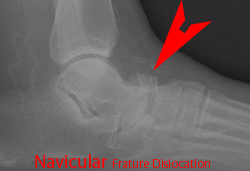
Sub-talar and forefoot dislocation
- Reduce immediately under Entonox ± IV Morphine and Midazolam (sedation sheet)
- Urgency = prevent skin overlying head of talus becomes ischaemic
- Refer to the on-call Orthopaedic Team
Lis-Franc fractures
Clinically
- Suspect injury if point tenderness over midfoot, or laxity between 1st and 2nd MT’s
Radiology
- > 1mm gap between adjacent bases of 1st and 2nd MT’s
- The six bone tarsometatarsal complex is known as the lis franc joint
- Uncommon, but up to 20% are missed
- Force of injury variable and can be minor rotational to severe axial load
- In most injuries involve disruption of the joint and associated fractures of metatarsals, cuneiforms and cuboids
- A fracture at the base of the 2nd metatarsal is pathogmonic of disruption of the ligament complex.
Types of Lis-Franc fractures
- Divergent: metatarsals splayed both medially and laterally - usually between 1st and 2nd MTs
- Isolated - one or more MTs are displaced from the rest
- Homolateral - all 5 MTs are displaced in the same direction either laterally or medially
Isolated fractures of the cuboid and cuneiform bones are rare and an associated injury to the lis franc joint should be sought
Management (thus why important to identify)
- Frequently require open reduction and internal fixation or Kirschner wires
- In interim, whilst waiting on orthopaedic opinion, should be immobilized in a below knee back slab and have hourly neurovascular obs due to the risk of swelling and compartment syndrome – (especially if crush type injury)
Complications
- Dorsalis pedis artery injury (double check pulse & perfusion)

Avulsion # base of 5th metatarsal
- Tubigrip [Bestbets] rather than plaster
- Elevation when not walking on it, exercises
- Stick or crutches
- Review in clinic only if difficulty mobilising
- POP only if patient unable to weight bear at all

Jones Fracture
- Transverse fracture of shaft of little metatarsal
- Very different to pull off fracture as above
- Unstable as peroneus (brevis) tendons distract fracture & mal/non union likely
- Treat in POP and refer VFAC

Other metatarsal fractures
- Ice, elevation and exercises. POP may be helpful if multiple fractures
Toe fractures
- If compound treat as for compound fractures plus soft footwear
- Fractures of the Hallux involving the articular surfaces require Fracture Clinic (CUH VTAC)
- Otherwise follow-up in the ED clinic or by GP
Thromboprophylaxis
In patients immobilised in leg casts:
- Consider prophylactic anticoagulation (LMWH) if high risk of VTE or prior DVT[BestBets]
- CUH EM and Orthpaedic divisions have reviewed the literature
- Prophylactic anticoagualtion is not required those pateints discharged in a splint but should be considered in all in PoP
Links
- EMed VTE Thrombophylaxis in leg PoP
- IAEM Policy on Thromboproplylaxis in lower limb injuries 2019
- Patient info. on thromboprophylaxis post leg immobilistation
- Thromboprophylaxis in lower limb immobilisation after injury (TiLLI). EMJ Journal Jan 2020, 37 (1) 36-41; DOI: 10.1136/emermed-2019-208944