Trauma call criteria:
Please contact the Emergency Medicine Consultant or Registrar if:
Mechanism
- MVC > 60km/hr
- Motor / cyclist impact > 30km/hr
- Pedestrian impact > 30km/hr
- Ejection from vehicle
- Prolonged extrication (>30min)
- Explosion
- Fall from > 5M height (may be less in a child)
- Major Burns
Vital signs
- Resp. rate <12 or > 24/min
- O2 Sats < 90%
- SBP < 90mmHg
- Pulse >124/ min
- GCS ≤ 9
Penetrating
- All penetrating injuries to the neck
Pregnancy & Trauma
- Pregnant patient ≥20 weeks gestation with ruptured membranes &/or PV bleeding &/or
Fetal heart rate < 100 bpm
Muitiple patients
- When ≥3 ambulance-borne trauma patients are expected from the same incident
Paediatric
- Vital signs in children outside 1 standard deviation of normal for that age
- These patients should be assessed initially in the Resuscitation Room on arrival
- Please note that, whilst these criteria are absolute for calling for senior assistance, there will be many trauma victims not covered here (e.g. the athlete with a pulse rate of 90, which is double their resting pulse rate) for whom you should also seek advice sooner rather than later

Management of Multiple Trauma Patients in CUH
- Please contact the on-call consultant in emergency medicine for all trauma cases with a CRAMS score of 8 or less
- When there is controversy or debate over which service should take primary responsibility for the patient, the senior emergency medicine doctor (Consultant or Registrar) should make the final decision about which service the patient is admitted under
- There has to be one main consultant, as above, but surgeons or other specialties who are involved in the patient's care should also be listed so that there is a clear chain of command for all involved in that person's care
- There has to be more registrar-to-registrar or consultant-to-consultant discussion of these cases
At CUH
- 300 people are assessed annually for multisystem trauma
- Many of these ultimately prove to have significant injury
- Multiple trauma is defined as an Injury Severity Score (ISS) >15
- But patients with an isolated femoral fracture face a mortality of up to 10%
- The ambulance service work to guidelines as to potential for multiple trauma in a patient
CUH, MUH, Mallow General Hospital
The first priority for a doctor receiving a case of possible multiple injury is adequate preparation. This includes calling for help. Familiarise yourself with the Resusc room and the resources available in it.
- The priorities of care are the ABCDEs
- Call an anaesthetist if the senior EM registrar is not RSI trained
- Spinal precautions continued throughout the patient's stay or until clearance by the most senior, appropriate, doctor is given
- All patients should be oxygenated with Hi Flow oxygen through a non-rebreathing mask. Oxygen saturations and respiratory rates should be monitored. Check tracheal position and air entry in both lung fields. Ventilate if necessary
- Consider bedside FAST/EGLS ultrasound
- Check pulse and BP. Stop obvious bleeding. Secure IV access with 2 large bore (16G) cannulae. Take bloods at this stage. Start warmed fluid replacement with crystalloid (saline or Hartmanns) or blood (please see massive transfusion protocol)
- All patients have a back as well as a front - log roll all patients
- Cross match, FBC and U&E, coag, Blood gases etc
- Consider MTP
- No life saving (including going to the operating theatre) intervention should be delayed to undertake investigations
- Consider "Pan-scan" if clinical situation allows. Beware the 'Donut of Death'
- Further investigation will be as determined by the patient's presentation and condition
- Clearly record procedures "To Be Done", e.g. "Cervical Spine Not Cleared", "Secondary Survey Incomplete"
The Emergency Department adheres to ATLS ethos and principles.
- Rapid primary survey (Airway with Cx spine control, Breathing, Circulation)
- Resuscitation
- Secondary Survey
- Safe transfer to definitive care
Tranexamic acid ( TXA )
- More on TXA in trauma
- TXA should be considered in in adult trauma patients at risk of significant bleeding
- TXA loading dose 1 g over 10 min then infusion of 1 g over 8 hours
Lactate
- Please record lactate / pH early in the resusciation
- ↓pH or ↑ lactate are poor prognositc features and should alert clinicians to active haemorrhage control (jtrauma/Abstract/2012/06000)
Links
Links CUH
- Trauma Triage (qpulse PPG-5), local copy
- Trauma Transfer/Egress (qpulse), local copy
- Trauma Triage Tool, local copy
- Trauma Reception (qpulse PPG-6), local copy
- Trauma MTC OP Policy (qpulse PPG-7), local copy
- Trauma Rehab. Needs Assment (qpulse PPG-3), local copy
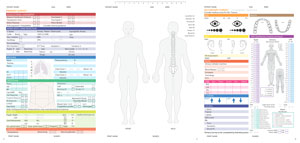
- Trauma TraumaDoc (IAEM site), local copy page A, page B
- Trauma Team Leader (TTL) checklist