Indications for nasal or Full face NIV
Based on the 2008 BTS Guidelines: NIV in COPD
Hypercapnic respiratory failure during an acute exacerbation of COPD with:
- VBG pH <7.35
- VBG PaCO2 >6kPa (if acute onset)
- Check ABG PaCO2 only if VBG CO2 high
- Tachypnoea >23 breaths/min
Uses
- Acute hypercapnic respiratory failure (e.g. in acute exacerbations of COPD)
- Cardiogenic pulmonary oedema
- Resp. failure in immunocompromised (e.g. LRTI)
- Neuromuscular disorders (respiratory failure)
- Asthma (selected cases only - senior decision)
Contraindications
- Facial trauma/burns
- Recent facial, upper airway or upper GI tract surgery
- Fixed obstruction of the airways
- Inability to protect airways or excessive airway secretions
- Life threatening hypoxaemia
- Undrained pneumothorax
- Impaired consciousness or confusion/agitation
- Vomiting
Assessment
- Full medical assessment
- Blood gases: pH 7.25 – 7.35; high PaCO2
- Optimal medical treatment not successful
- Consider commencing NIV
- Have a plan for if NIV fails
- Aim for ↑pH, ↓PaCO2 and ↓RR after 1hr of NIV
- ?Chance of failure – high Apache score, poor nutritional status, confusion/impaired consciousness
- Inform ITU of decision to commence NIV
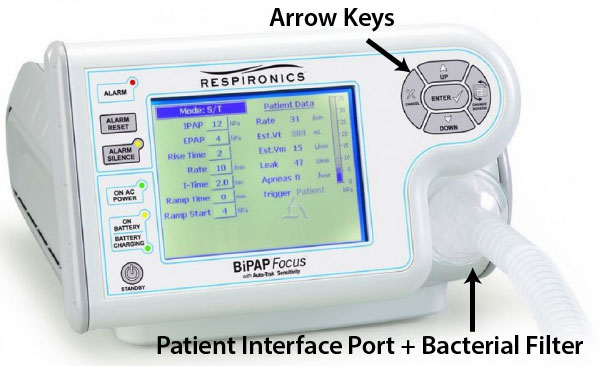
Setting Up (Bipap Focus)
- Senior decision maker to commence NIV
- NIV machine (Bipap Focus in CUH) + tube + CO2 exhalation port + mask + head-cap
- On the BiPaP focus machine, the O2 tubing can be attached into the port on the face mask or beside the exhalation port
- Set EPAP at 4 – 5 cm H2O and IPAP at 10 cm H2O
- Set back-up breathing frequency to 8 – 10 breaths/minute
- Select appropriate size mask (full face in preference to nasal) to fit patient
- Explain procedure to patient
- Hold mask in place to allow patient to familiarize themselves
- Attach pulse oximeter
- Commence NIV, holding mask in place initially
- Secure mask in place with straps/headgear to prevent leaks – do not attach too tightly!
- Reassess patient after a few minutes
- Check for leaks and refit mask if necessary
- Add O2 to maintain SpO2 >85%
- Instruct patient how to remove the mask and summon help
- Increase IPAP gradually up to about 12 - 15 cmH2O over 1 hr
- Clinical assessment and, if appropriate, check ABG at 1 hour
- If procedure fails, institute alternative management plan
COPD Patients in MUH ED
In MUH, COPD (in contrast to LVF patients) can be non-invasively ventilated using the guidelines shown right.
Initiating NIV
- Commence BiPAP at IPAP 10cm H20 / EPAP 5cm H20
- Increase FiO2 to improve O2 saturation to >90%
- Repeat gases after 1 hr of NIV treatment
- Titrate IPAP
- if pH<7.35, respiratory rate >25/min, PaCO2>6 kPa or persistent use of accessory muscles
- Titrate EPAP if if persistent hypoxia
- Titrate in increments of 2cm H20 to peak IPAP 20/EPAP 8
- Repeat blood gases after 4 hrs of NIV; titrate pressures as above
- NIV should be used for a minimum of 16 hours / 24 hours initially, reducing to 12 hours on Day 2, and 8 hours on Day 3 as the clinical setting permits
Full ventilation reconsidered if:
- pH<7.2
- pH 7.2 - 7.25 on two occasions 1 hr apart
- Hypercapnic coma GCS <8 and PaCO2>8 kPa
- PaO2<6 kPa despite maximum tolerated FiO2
- Cardiorespiratory arrest
Treatment failure
- Is medical treatment optimal?
- Is physiotherapy needed (particularly for sputum retention)?
- What complications have developed (beware PTX or aspiration etc.)
- Check the pressures actually being achieved ( visible on the screen of the Bipap Focus)
- If PaCO2 remains high or pH ↓:
- To much O2? Maintain SpO2 between 85% to 90%
- Excessive mask leakage?
- Is circuit set up correctly?
- Is patient synchronising with ventilator – adjust breathing rate and/or inspiratory and/or expiratory trigger
- Is re-breathing occurring? - Check patency of expiratory valve (if fitted). Consider increasing EPAP
- Is ventilation adequate – ?increase IPAP (increments of 2cm H2O to alleviate resp distress)
- If PaCO2 improves but PaO2 remains low:
- Increase FiO2
- Consider increasing EPAP by increments of 2cm H2O. NB keep difference betw. IPAP and EPAP ≥ 6 cmH2O - so you may need to also increase IPAP
Aims of NIV
- Deal with acute phase of respiratory failure
- Attempt to stabilise patient’s condition
- Contact ITU Registrar prior to transfer to medical ward
- Treatment failure warrants ITU admission
Infection control
- Disposable masks and exhalation ports should be disposed of
- Headgear should be washed in a washing machine – be careful with the Velcro straps
- Use a bacterial filter between the tube and the BiPaP machine to reduce contamination risk to machine
References
- 2008 (October) BTS GUIDELINE. NIV - COPD
- CUH policy on NIV (abbreviated version) April 2015
- Print copy setting up BiPAP Focus NIV machine
- Setting up Nippy 3 NIV machine (print (PDF) version)
Links
- Triology Hood set up
- Triology face mask set up
- Airvo set up
- Triology Setting Guide
- Philips Trilogy 202 - Non Invasive, Invasive Ventilation